At first, there so much noise. Phones ringing, kind and supportive messages flooding in. Appointment after appointment, preparation for surgery after surgery. Fitting it all in becomes a full time job. Information is a flood, coming at you faster than you can process it, like drinking from a fire hose. People are everywhere, offering a … Continue reading The Loneliness Experienced During Forever Cancer Care
Chronic v. Terminal
There’s been several articles recently labeling Stage IV Metastatic Breast Cancer (MBC) as a chronic disease sponsored by and including various non profits. Ironically none of the articles I’ve seen provides justification or basis for this claim and none cite to medical doctors or scientific proof. Instead of actual evidence or attempting to explain, the … Continue reading Chronic v. Terminal
Navigating Grief and Support for MBC Patients
In my circles of good friends living with Stage IV Metastatic Breast Cancer (MBC), there is a great deal of suffering at present and that weighs on all of us. It is not abnormal to get on a zoom call ostensibly about the "business" of advocacy and talk mostly about these personal struggles because we … Continue reading Navigating Grief and Support for MBC Patients
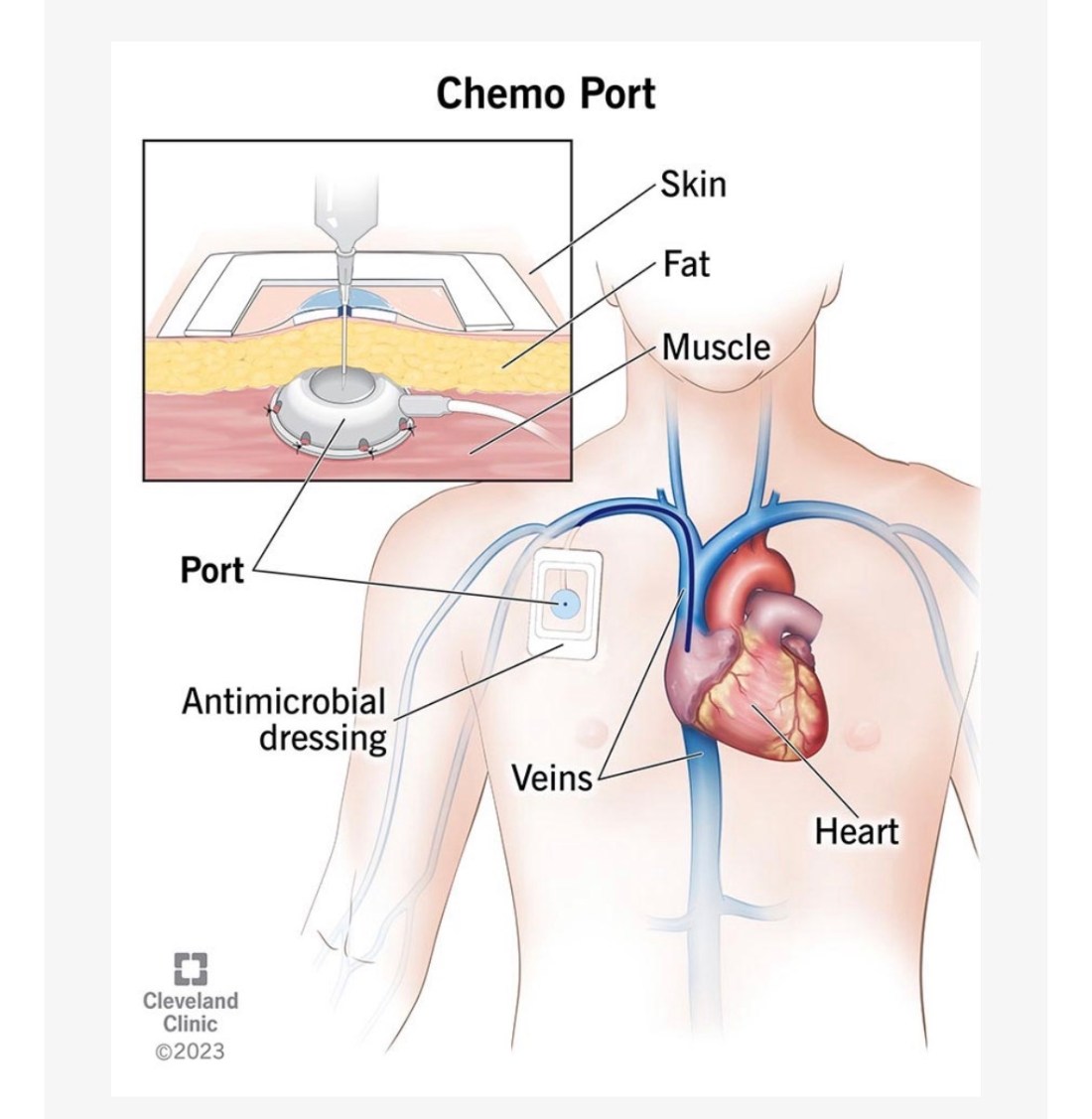
Things to know when you are getting a port, from a patient’s perspective
After receiving three different ports after my de novo Stage IV Metastatic Breast Cancer (MBC) diagnosis in 2017, I've collected a few important things to think about along the way that I'd like to share. Not everyone living with MBC has a port and not all patients living with MBC desire one. It is important … Continue reading Things to know when you are getting a port, from a patient’s perspective
Clinical Trials, Part II: Informed Consent
During the 2025 San Antonio Breast Cancer Symposium (SABCS), I had the privilege of participating in a panel discussion that was a collaboration between the Alamo Breast Cancer Foundation, the Metastatic Breast Cancer Alliance (MBCA), the American Association of Clinical Research (AACR) and the Advanced Breast Cancer Global Alliance (ABCGA). Dr Fatima Cordoso and Teri … Continue reading Clinical Trials, Part II: Informed Consent
ReBlog: Journeying Beyond Breast Cancer’s Weekly Round-Up
Time for this week’s round-up of the best of the blog posts which I’ve read over the past week. These are the posts that have moved me, taught me … Weekly Round-Up
Finding Clinical Trials: A Patient’s Guide
During the 2025 San Antonio Breast Cancer Symposium (SABCS), I had the privilege of participating a panel discussion that was a collaboration between the Alamo Breast Cancer Foundation, the Metastatic Breast Cancer Alliance (MBCA), the American Association of Clinical Research (AACR) and the Advanced Breast Cancer Global Alliance (ABCGA). Dr Fatima Cordoso and Teri Pollastro … Continue reading Finding Clinical Trials: A Patient’s Guide
ReBlog: Weekly Round-Up from Journeying Beyond Breast Cancer
Time for this week’s round-up of the best of the blog posts which I’ve read over the past week. These are the posts that have moved me, taught me … Weekly Round-Up
Navigating Life’s Turmoil: A Call for Connection and Action
When we add up all of the chaos, only exacerbated by the perpetual news cycle, the burden of trying to find truth when no one gives us everything, it is entirely reasonable to feel paralyzed, to feel as though all hope is lost, to not know where to turn. Whenever I turn on the news, … Continue reading Navigating Life’s Turmoil: A Call for Connection and Action
When a door closes, open a window … but what about when you run out of windows?
In this clumsy metaphor, the doors and windows are treatment options for Stage IV Metastatic Breast Cancer (MBC) and so many of us only have a finite number of treatments before this terminal diagnosis completes its trajectory and ends its own existence and the host. Reaching the end of a treatment option and contemplating the … Continue reading When a door closes, open a window … but what about when you run out of windows?