One of the aspects of living with Stage IV Metastatic Breast Cancer (MBC) that is often difficult to explain to people who have not experienced MBC or other life-limiting diagnoses is the stress and strain of making many treatment decisions over the time that we live with the disease. I wrote a post a few months ago, Xeloda and Topical Heparin, about the various lines of treatment I’ve been on since my de novo MBC diagnosis in 2017 — I do think that the total lines of treatment is five (5), but we’ve made adjustments within those lines as well. We’ve had to make a lot of decisions over the past six (6) years and while I can’t say that I have everything figured out, I’ve learned a little about how to navigate the changes that happen so very often.
Presently, we are in the throes of making a treatment decision again because the PET/CT I had at the Mayo Clinic in Jacksonville last Friday demonstrated that Xeloda by itself is not sufficient to keep the cancer in my body in check. A silver lining is that the Brain MRI demonstrated there are no mets there, which was a huge relief.
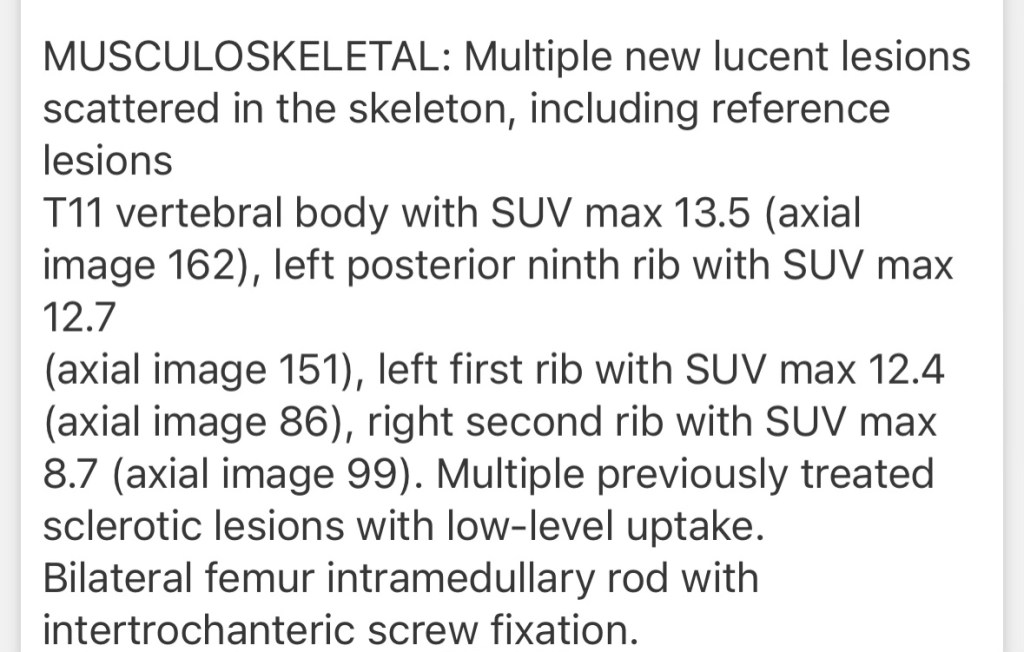
Here’s the pertinent language from the PET/CT:
I met with my Mayo oncologist via telemedicine this morning and am meeting with my local oncologist on Thursday, plus reaching out to those docs that I consider my “second opinions,” even though there are more than 2. Yes, I realize this might seem like overkill and I do have some ideas in my mind already about what we should do, but I really really really like having lots of smart people thinking about these serious decisions. If I could manage even more docs, I probably would, but five (5) is probably my limit.
Anyway, lots of changes coming and while I know I’ve written before about making these decisions (see this post), I wanted to lay out how I’m making this decision and would love to hear from each of you any tips or tricks you’ve employed as well.
First, as I attend conferences, talk to people, and generally live in and around MBC, I have a running list of all the medications I hear about along with what I learn from other patients about how they handle the medication. This is a pretty long list now, but I’m always updating and adding to it. Yes, the new medications go on that list, including the ones I’m watching to see when they get approved, but I also make sure to include those medications that aren’t so new. I’ve learned over time that the medical teams usually have a lot of tricks to deal with the older medications but are having to learn the newer ones right along with the patients. Just one more thing to think about.
Second, I’ve established and maintained relationships with a variety of medical oncologists. This can be a lot of work since I am the one sending my PETs or other medical records to each of these other doctors and meeting with them has necessitated some travel, although I try to do tele-medicine as often as possible. Those relationships, though, allow me to reach out in times like these to get a variety of input. And, yes, I have had to deal with my insurance company covering those appointments and I’d be happy to talk with anyone who is interested in figuring out how to do this.
Third, every time there is progression or my tumor markers are rising, I ask for liquid and tissue biopsies. We haven’t always gotten great information from the liquid biopsies, but my first instinct is to make sure we have sufficient information about how the cancer is changing and mutating so that we can make the best decision possible about a treatment. Having had a lot of bone mets over the years and not many visceral mets, getting tissue biopsies has been difficult at times.
Fourth, whenever there is progression, I always ask which other professionals I should/could meet with. For example, since some of those new or newly active mets are showing a pretty high SUV level (meaning they are highly metabolically active), I’ll be meeting with a radiation oncologist to see if radiation is a good idea.
Fifth, whenever I’m considering a medication, I always reach out and ask people who have taken the medication about their experiences. While I am fully aware that everyone is different, having information in my list as to the side effects and how people manage them is really important to me. I can read all the lists or hear from doctors about what they think could happen, but the real world experiences are so much more valuable in my experiences thus far.
Sixth and finally, I work with my husband to look at how a medication is going to affect/change our household and how we might address those things proactively. For example, the chemo regimen I will likely be utilizing is given in a three week cycle. Since I know that the first week after the infusion is likely going to be when I’ll have the most fatigue and other side effects, my husband has reached out to his manager to ensure that he can work from home that week to be available. We’ve reached out to family and friends to solicit some extra help and I’ll be examining closely all those things that I do on a regular basis to evaluate what I can step back from and what is necessary and where I can get backup.
So, stay tuned for the decision after I’ve made the rounds to the different doctors and talked to everyone I can find who might have ideas.

Good luck. I feel like I am making big decisions at times when I am emotionally and cognitively limited. I admire your energy, hope you get a good plan.
LikeLiked by 1 person
It’s so true, we so often have to make the biggest decisions when we’re the least equipped to do so.
LikeLike
This is a distressing but uplifting post, Abigail. And—as always—your sharing your options and thought processes means helping so many others while you’re making these difficult decisions for yourself and your family.
It’s encouraging to be reminded of the informational bank account you’ve accrued that will assist you now.
Sending you my most positive healing thoughts and my love. Annie
LikeLiked by 1 person
Count on me for some meals during the upcoming treatment! 🍲❤️
LikeLiked by 1 person
Thank you so much! 🙂
LikeLike
Thinking of you.
LikeLiked by 1 person
Thank you for sharing. I hope you have a plan in place soon and that it makes those cancer cells start being lazy AF
LikeLiked by 1 person
From your mouth to God’s ears!!
LikeLike
Abigail you have helped me (and all Stage IV patients) immensely by describing your process when facing progression/decisions. It seems all of us would benefit from being more proactive. I know that when I have, I have had more confidence in my choices and calmness in what’s ahead. I send you all the best and many thanks for this blog and the good it does.
LikeLiked by 1 person
Appreciate you reading and commenting! Making so many decisions is something we all face and yet it’s not a hot topic of conversation. I’m so glad my list helps you. 🙂
LikeLike
Hi Abigail,
I’m sorry to hear about the progression. Good luck making these difficult decisions about what’s next. In your corner. Always. x
LikeLiked by 1 person
Thank you so much!! Appreciate your support, always. ❤️
LikeLike
It amazes me the resources you/we have access to today, compared to when my mother had MBC. Then, Mom and Dad did the best they could.
LikeLiked by 1 person
So true and people like your family are the ones we’ve learned from! We’re all doing the best we can.
LikeLiked by 1 person
I know. I miss my Mom—she passed away October tenth, 1990, I think.
LikeLiked by 1 person
My condolences. Such a hard thing.
LikeLiked by 1 person
Thank you. It was harder earlier on.
LikeLiked by 1 person
I’m so sorry you are dealing with more active disease, but so proud of you for how well you handle it and use your experience to help others. Please know I am here and I can help out if you need anything at all. As opposed to when you were farther away.
LikeLiked by 1 person
appreciate you, my friend. We’re still in the throes of figuring things out, so will let you know when I know …
LikeLike